The unwinding of Medicaid coverage due to eligibility reviews has affected millions of Americans, leading to disruptions in healthcare access and treatment. Justin Gibbs, a father of four from Ohio, experienced a week without essential medications for his high blood pressure after losing Medicaid coverage. While he was able to secure new prescriptions when his Affordable Care Act policy kicked in, many others who were disenrolled faced struggles in regaining coverage, leading to fears about their physical and mental health. The process has highlighted the challenges faced by disenrolled individuals in maintaining their health and well-being.
The impact of Medicaid disenrollment has been significant, with nearly a quarter of adults reporting being uninsured after losing coverage. While some were able to regain Medicaid or secure coverage through other sources, such as an employer or Affordable Care Act exchange, many faced gaps in care and medications during the transition period. The disruption in coverage has caused considerable concern and worry among those affected, underscoring the need for more comprehensive tracking and support for disenrolled individuals.
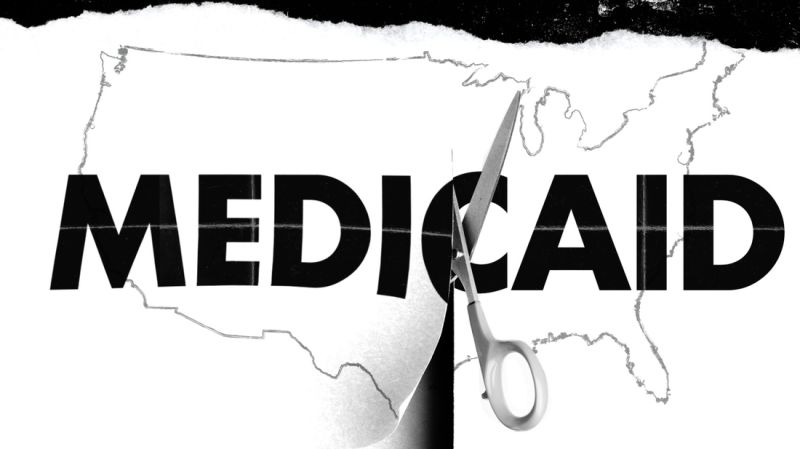
The Covid-19 pandemic provided temporary relief for many Medicaid enrollees, delaying the renewal process and preventing disenrollment for several years. However, as eligibility reviews resumed, millions of individuals found themselves at risk of losing coverage, with procedural reasons cited as the primary cause. This has raised concerns among federal officials and advocates about the potential for eligible individuals to become uninsured due to administrative hurdles and complexities in the renewal process.
The renewal process for Medicaid coverage has posed challenges for many enrollees, with long wait times for assistance and confusion over required documentation. Despite efforts to maintain coverage, some individuals faced difficulties in navigating the renewal process, particularly those with limited internet access or in states with additional documentation requirements. The need for assistance and support in renewing coverage has been evident, highlighting the importance of streamlining the process and providing resources for disenrolled individuals.
Individuals like JP Peters, a Florida resident who relied on a retired nurse friend for assistance in enrolling in Medicare, faced uncertainties and delays in securing coverage during the renewal process. The anxieties and challenges associated with potential loss of coverage have been felt by many disenrolled individuals, leading to delays in necessary medical treatment and concerns about healthcare costs. While some were able to navigate the renewal process with assistance, others faced obstacles that impacted their access to care and medications.
Overall, the Medicaid disenrollment process has revealed gaps in coverage and support for individuals transitioning between programs or experiencing changes in eligibility. The complexities of the renewal process, coupled with administrative barriers and procedural challenges, have highlighted the need for improved coordination and assistance for disenrolled individuals. Addressing these issues will be essential in safeguarding the health and well-being of vulnerable populations and ensuring continuity of care for those relying on Medicaid for essential healthcare services.